The Family Caregiver’s Guide to Lung Cancer

Approximately 43.5 million Americans are informal caregivers, meaning they provide unpaid medical care to a child or adult. Of these caregivers, 85% care for a family member — most commonly an aging parent.
Being a caregiver for a family member with lung cancer means you’ll need to wear many hats. Your responsibilities may include staying on top of medication and nutrition, being a source of emotional support, helping a patient transition to hospice care and more. Throughout your caregiving experience, you’ll also need to remember to take the time to care for yourself both physically and emotionally.
The best thing you can do as a lung cancer caregiver is educate yourself. Become familiar with your loved one’s cancer type — whether it’s small cell lung cancer, non-small cell lung cancer or another cancer that affects the lungs such as lung sarcoma, lung lymphoma or mesothelioma. Learning about the nature of the patient’s cancer will help you make better-informed caregiving decisions.
Caring for a Lung Cancer Patient
As a caregiver, it’s your job to stay on top of doctor’s appointments, medication dosages, managing treatment side effects and ensuring the patient gets proper nutrition. The more you understand your loved one’s condition and the treatment they’re receiving, the better equipped you’ll be to help them through this difficult time. Here are some first steps that caregivers should take:
- Get a solid diagnosis — usually from a biopsy — from a lung cancer specialist
- Read up on the specific skills you’ll need to treat someone with lung cancer
- Discuss a plan of care with family and close friends
- Organize your research in a binder and make copies for any other caregivers
The next step in lung cancer caregiving is understanding treatment options, which typically include a combination of chemotherapy, radiation and surgery. Depending on the type and stage of the lung cancer, treatment and recovery may span months or years. After treatment, regular follow-up appointments are required, so it’s best to be prepared for the long haul.
Chemotherapy and Radiation for Lung Cancer Patients
Chemotherapy kills cancer cells and stops them from spreading, but it may also affect normal cells. It is administered in cycles, and each cycle lasts three or four weeks. Late-stage patients may need up to six cycles.
Depending on the dosage and other medical issues the patient has, chemotherapy may cause some side effects. Caregivers should familiarize themselves with the following common side effects so they can be prepared to handle them effectively:
- Anxiety and mood changes
- Bruising
- Fatigue and tiredness
- Hair loss
- Increased risk of infection
- Mouth dryness and sores
- Stomach problems
Radiation for lung cancer patients is aimed at the chest and abdomen, which may cause the following site-specific side effects:
- Skin peeling and blisters
- Breast soreness
- Cough
- Difficulty swallowing
- Shortness of breath
- Shoulder stiffness
In addition to chemotherapy and/or radiation, the patient may need surgery as part of their treatment process.
Before and After Lung Cancer Surgery
Surgery for lung cancer or mesothelioma may be necessary to remove or shrink a tumor, remove a lung via a lobectomy, or to ease a patient’s symptoms. Keep in close communication with the patient’s team of surgeons and oncologists to determine how you can provide the best care both before and after surgery.
Depending on the procedure and treatment, you may need specialized equipment such as an oxygen tank, ventilator or spirometer to measure the volume of air inhaled and exhaled. Make sure you know how to safely operate any necessary equipment.
It may take one or two months to fully recover from lung cancer surgery. If the patient smokes, encourage them to reduce or stop cigarette usage at least a month before the surgery. This will help them heal more quickly and reduce the risk of postoperative complications. You should also encourage light exercise like a daily walk to increase lung capacity before surgery.
After the surgery, it’s best to follow the doctor’s recommendations as closely as possible. You’ll want to encourage the patient to discontinue narcotic painkillers as soon as possible to lessen side effects like constipation and nausea. You should also monitor the patient’s activity to make sure they’re not doing anything their doctor told them to avoid, such as driving or lifting anything heavy. You’ll also want to monitor the surgical wound or incision and keep an eye out for signs of infection such as swelling, redness or drainage.
In addition to medication and rest, a key part of postoperative recovery is making sure the patient gets adequate nutrition.
Patient Nutrition
One common issue among lung cancer and mesothelioma patients is unintended weight loss. According to the Journal of Oncology Practice, 34% of cancer patients experience weight loss before they are diagnosed.
Stomach problems, including nausea, vomiting and constipation, are common side effects for lung cancer patients. Because of this, it is sometimes difficult for patients to muster up an appetite. However, ensuring proper nutrition throughout treatment is crucial in helping a patient avoid weight loss and strengthening their ability to heal and recover from surgery. When you’re caregiving for a lung cancer patient, ensure the following:
- Before treatment: Stave off weight loss by focusing on calorie-rich foods high in healthy fats and protein, such as nuts, avocados, whole grains and legumes.
- During treatment: Patients may have a diminished appetite, so continue focusing on calorie-rich foods to pack as much nutrition into each bite as possible. If the patient can’t tolerate three larger meals per day, encourage them to have a small snack every 60 to 90 minutes.
- After treatment: Once the patient begins to regain strength, their body can make better use of protein and calories. If their weight has stabilized, incorporate fruits and vegetables to aid in the recovery and strengthening of their immune system.
If the patient is showing changes in their ability to eat or if you have any questions about their nutritional needs, always consult their doctor or dietician.
Special Caregiving Circumstances
While the symptoms of lung cancer are largely universal, there are extenuating circumstances that may present unique challenges and additional considerations. Two of the most common special caregiving circumstances include long-distance caregiving and caregiving for a veteran with lung cancer.
Long-Distance Lung Cancer Caregiving
If you travel an hour or more to care for a patient, you’re likely experiencing a set of challenges unique to long-distance caregiving. According to the National Center on Caregiving, approximately 15% of caregivers are long-distance caregivers. To maximize the quality of care your loved one receives, consider the following action items:
- Research resources close to the patient. Family Care Navigator and Eldercare Locator are great tools to find help.
- Form a solid understanding of the patient’s current state of health. This will help you understand their needs and anticipate any issues. Put together a notebook of references and important contact information and update it frequently.
- Make the most of your visits. Reach out to the patient ahead of time to see what they would like to do during your time together. If they have a primary caregiver, set up a time to talk about how you can be most helpful.
- Stay connected. Ensure the patient has a cell phone and can easily call you if they have questions or just want to talk. If they live in a nursing home, see that they have a private line installed in their room.

Don’t underestimate the power of a simple phone call. The best thing you can do when you’re far away is make yourself available for the patient and provide support in any way possible despite your distance.
Lung Cancer Caregiving for Veterans
Lung cancer is especially prevalent among veterans. According to a 2012 VA study in Military Medicine, lung cancer is the second most frequently diagnosed cancer among VA patients. Additionally, veterans make up about 30% of mesothelioma legal cases. If you’re caregiving for a veteran, you may have access to additional resources through the U.S. Department of Veterans Affairs.
VA Health Care
If the veteran served in the active military service and was not dishonorably discharged, they may qualify for VA health care benefits. This includes — at little to no cost — medical equipment, home health care, prescriptions and more. To apply for VA health care benefits, you’ll need proof of discharge, income information and current health insurance information. You’ll apply via the VA website.
Lung Cancer and VA Disability Benefits
If the patient can prove that their lung cancer was connected to an injury, illness or event during their service, they may also qualify for VA disability benefits. Common causes of lung cancer during the military include exposure to Agent Orange, radiation and asbestos.
The VA typically gives service-related cancer a 100% disability rating, meaning the patient will earn the highest level of benefits. These benefits will continue until six months after a successful treatment program. You can see the VA’s disability and compensation rates here.
Facing the End of Life
If the patient’s cancer diagnosis is terminal, there are certain things you’ll want to prepare for. From financial and legal considerations to hospice and palliative care and emotional support, helping your loved one prepare for the end of life can be difficult. Conversation avoidance is common — approximately 80% of American families haven’t discussed end-of-life plans. Having the conversation early and staying educated on what you need to do will help the process go as smoothly as possible.
Palliative Care and Hospice
From a treatment perspective, palliative care and hospice are often implemented near the end of life. However, a primary difference between the two is that palliative care can be used any time, even with curable cancer, and hospice care is designed for people in the last six months of life.
Palliative care focuses on the management of pain and other symptoms of cancer to improve the patient’s overall quality of life. Surgery, radiation, chemotherapy and medications that aim to relieve pain and other cancer symptoms may all fall under the umbrella of palliative treatment. If a patient begins palliative treatment soon enough, they may be able to live a longer and more enjoyable life.
Once a patient is given six months or less to live, you and your family may want to consider hospice care. Hospice focuses on preserving a patient’s quality of life and easing symptoms. Depending on the level of care needed, you may opt for basic at-home care or more intensive inpatient care at a facility.
Hospice care involves a team of doctors, nurses, specialists, counselors, social workers and more. For lung cancer specifically, hospice may also include facilitated breathing.
When deciding on a hospice program, you’ll want to consider the following action items:
- Obtain a referral from your doctor. You’ll need the patient’s oncologist to sign paperwork that confirms they are eligible for hospice care.
- Determine the quality of care. Look for hospice programs that are certified by Medicare, meaning they meet a specific standard of care. With over 4,700 hospice options in the U.S., make sure you have a good understanding of the type of care your loved one will receive by interviewing the facility’s medical director.
- Tour the facility. If you opt for inpatient care, you’ll want to tour the facility and be sure you’re confident in their experience with lung cancer patients.
Preparedness
If the patient becomes too sick to make decisions about their care, they’ll want to have some measures in place to ensure they are taken care of and that their wishes are fulfilled. As their primary caregiver, you’ll likely be responsible for helping the patient set up the following:
- Advance Directives: These are legal documents that communicate your treatment preferences in case you aren’t able to. Common considerations for lung cancer patients include whether or not they wish to use a breathing machine or be resuscitated.
- Health Care Proxy: This is the person who will follow the advance directives and communicate with doctors on the patient’s behalf. As their caregiver, you should be prepared for the possibility that they may choose you to be their health care proxy.
- Will: Make sure the patient has a written will that will decide how their property and assets will be distributed as well as who will care for children, if there are any. Without a will, these decisions are left to judges and state officials.
- Funeral Arrangements: Decide how the funeral costs will be covered and research funeral homes. Although it may be difficult, you should discuss with the patient if they want to be buried or cremated and if they have any wishes for the funeral ceremony.
In addition to end-of-life preparations, you’ll also want to have an emergency preparedness plan in place. You’ll want to be familiar with the nearest emergency room and have a list of doctor’s numbers to call in case the patient experiences sudden complications due to a procedure or medication side effect.
Caregiver Self-Care
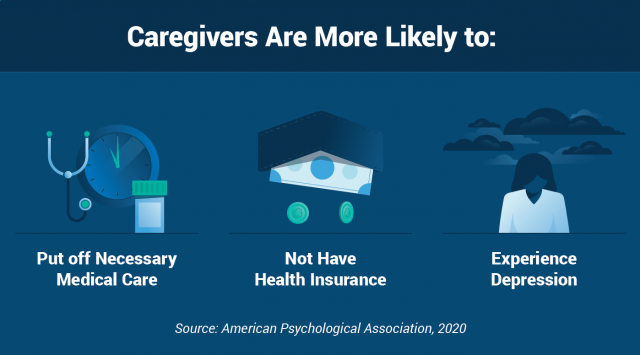
When your life revolves around caring for someone else, it’s easy to forget to care for yourself. One recent study from the American Psychological Association found that caregivers are more likely to neglect their own health by delaying necessary health appointments or not having health insurance. Another poll from the University of Chicago found that approximately one third of caregivers have skipped a routine physical or dental appointment, have failed to schedule much-needed care or have failed to refill a prescription.
In order to give the best care possible to your loved one, you need to make sure that you’re in the best possible condition yourself. This means, at the very least, taking care of the following:
- Keep up with your own doctor appointments. Stay on top of screenings, vaccinations, eye appointments, dental cleanings and any other doctor-recommended treatments.
- Stay in good physical shape. Aim for 30 minutes of light-to-moderate exercise each day. This will help you feel less stressed and give you more energy for your caregiving tasks.
- Establish a good sleep routine. Without eight hours of quality sleep, it may be more difficult to handle stressful situations or to remember important appointments or treatment details.
Your self-care regimen should also include caring for your mental health to avoid burnout — something that’s unfortunately common among caregivers.
Caregiver Burnout
As a caregiver, there may be times when you feel like you’ve failed. This may cause you to feel guilty or blame yourself. During these times, remember to be gentle with yourself and know you’re doing the best that you can. Acknowledge your strengths and all of the things you’ve learned and accomplished so far. Remind yourself why you took on this caregiving task in the first place.
Stay social during this time to ease feelings of isolation and hopelessness. Connecting with others in a similar situation can also help ease the burden of caregiving. Look for local or online support groups for people who have been affected by lung cancer.
Support Services
It’s crucial to remember that you’re not alone in your caregiving experience. If you’re feeling burdened by caregiving tasks, remember that you can offload and delegate certain tasks and routine chores to others who are willing to help. Here are some ways to lessen the burden of your caregiving load:
- Sign up for a healthy meal delivery service. You can stockpile meals in the freezer and save them for a busy day when you’re too tired to cook or do the dishes. Alternatively, you can ask loved ones to bring over homemade meals.
- Recruit a family member or trusted friend to take the patient outside, if they’re able. Use this as an opportunity to enjoy some alone time at home or to pursue a hobby.
- Hire a cleaning service to help with keeping the house tidy and fresh. This will help boost your mood and ensure an optimal environment for healing and well-being.
Additional Resources
In addition to practicing self-care and seeking out support services, explore the following resources on lung cancer and caregiving to improve your education and well-being as a caregiver:
Rosalynn Carter, former first lady and president of the Rosalynn Carter Institute for Caregiving, said in a written testimony, “There are only four kinds of people in the world. Those who have been caregivers, those who are currently caregivers, those who will be caregivers and those who will need a caregiver.”
Caregiving connects us all. Throughout the difficult times, remember that knowledge builds confidence. Keep learning about your loved one’s lung cancer and you’ll be prepared to handle anything that comes your way.

